In the First State of the Nation Address of His Excellency, Presidency, President Benigno S. Aquino III, to the Congress of the Philippines on July 26, 2010, the Department of Social Welfare and Development (DSWD) was directed to implement the National Household Targeting System for Poverty Reduction (NHTS-PR) that will identify poor families that most urgently need assistance.
In line with this, PhilHealth Board Resolution No. 1417, s. 2010 provides for the "adoption of the means test protocol of the National Household Targeting System for Poverty Reduction of the Department of Social Welfare and Development (DSWD) and be the source of all indigent families to be enrolled under the Sponsored Program of the NHIP.
The General Appropriations Act (GAA) for FY 2012 has provided budget amounting to P12.028 billion as "Subsidy for Health Insurance Premium of Indigent Families Enrolled in the National Health Insurance Program" under the Office of the Secretary of Health. It is also provided in the special provisions that it "shall cover the National Government subsidy for health insurance premium of indigents under the National Household Targeting System for Poverty Reduction of the DSWD." The Corporation through PhilHealth Board Resolution No. 1571, s. 2011 allowed the enrollment of all indigent families under the NHTS-PR of the DSWD under the Sponsored Program.
Since all identified Pantawid Pamilyang Pilipino Program beneficiaries are included in the NHTS-PR list of poor households of the DSWD, they shall, therefore, be enrolled and provided coverage under Sponsored Program Component the National Health Insurance Program (NHIP)
II. COVERAGE
All Pantawid Pamilyang Pilipino Program (also known as "Pantawid Pamilya") beneficiaries, and their qualified dependents, included in the list of poor households under the NHTS-PR of DSWD shall be entitled to all NHIP benefits in all health care providers accredited/contracted by PhilHealth.
III. ENTITLEMENT
All Pantawid Pamilya beneficiaries as Sponsored Program members under the NHTS-PR, including their qualified dependents, are entitle to the following NHIP benefits:
- Primary Care Package, as per PhilHealth Circular No. 10, s. 2012, with subject: Implementing Guidelines for Universal Health Care Primary Care Benefit I (PCB1) Package for Transition Period CY 2012-2013;
- All inpatient and outpatient care services;
- In addition, the Pantawid Pamilya beneficiaries and their dependents are entitled to the No Balance Billing Policy (NBB), as per PhilHealth Circular No. 11, s. 2011, with subject: New PhilHealth Case Rates for Selected Medical Cases and Surgical Procedures and the No Balance Billing Policy, which specifically states that no additioanl amount shall be charged to Sponsored Program members and/or their dependents who:
- are diagnosed with any of the 23 cases under case payment and admitted to non-private accommodation beds of government hospitals;
- have availed of outpatient surgeries, hemodialysis and radiotherapy in accredited non-hospital facilities, including free-standing dialysis centers (FSDCs) and ambulatory surgical clinics (ASCs); or those who utilized existing outpatient packages for TB-DOTS, Malaria, HIV/AIDS; and
- have availed of services under the Maternity Care Package (MCP) and the Newborn Care Package (NCP) in accredited MCP (non-hospital) providers.
IV. PANTAWID PAMILYANG PILIPINO PROGRAM ID CARD AS ACCEPTABLE PROOF OF ENTITLEMENT TO NHIP BENEFITS
The DSWD provides a unique Identification (ID) card to all primary beneficiaries under the Pantawid Pamilyang Pilipino Program. This ID Card shall be acceptable to establish eligibility to claim NHIP benefits, in lieu of the Health Insurance Card (HI Card) and/or Member Data Record (MDR) in the interim.
Sample Pantawid Pamilya Identification Card, is as seen below:
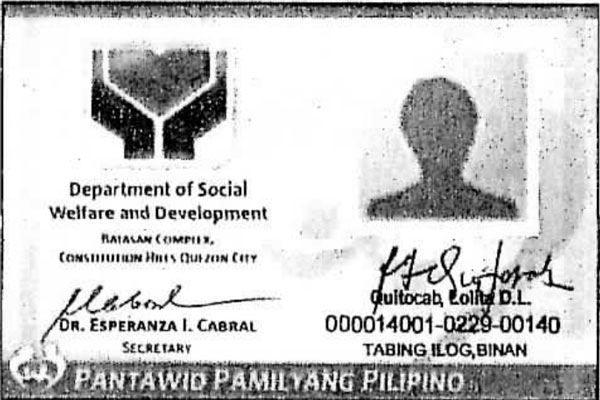
Pantawid Pamilyang Pilipino ID (front view)
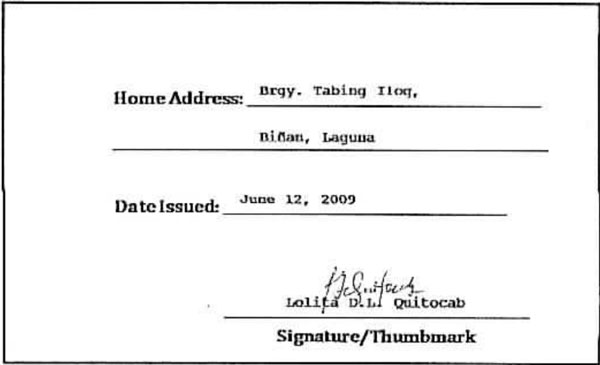
Pantawid Pamilyang Pilipino ID (rear/back view)
Upon presentation of Pantawid Pamilya ID Card, a Pantawid Pamilya beneficiary, either as Sponsored Program member or a as a qualified dependent, shall be entitled to all NHIP benefits in any health care provider accredited/contracted by PhilHealth.
- For Pantawid Pamilya primary beneficiary member-patients, no other supporting documents to establish eligibility shall be required from the member;
- For dependent-patients, aside from the aforementioned Pantawid Pamilya ID card, any of the following supporting document/s, whichever is/are applicable (pursuant to Section 10, Rule II, Title III, Implementing Rules and Regulations of the National Health Insurance Program, Republic Act No. 7875, as amended by Republic Act No. 9241):
- Marriage Contract/Certificate - for dependent spouse;
- Birth/Baptismal Certificate - for dependent legitimate, illegitimate, legitimated children;
- Court Order on Adoption - for dependent adopted children;
- Birth/Baptismal Certificate of the member and dependent parents - for dependent parents;
- Marriage Contract of the parent and stepfather/stepmother and birth certificate of the dependent stepchildren - for dependent stepchildren;
- Joint affidavit of two (2) disinterested persons and other relevant information (date of birth, etc.) attesting to the fact of the relationship of the dependents to the supposed member except the declaration of spouse;
- Certificate from the Department of Social Welfare and Development (DSWD) or Punong Barangay attesting to the fact of the relationship of the dependents to the supposed members;
- Any other valid ID or document acceptable to the Corporation, to wit but no limited to the following;
- Certification from DSWD or MSWD or Barangay that concerned dependent-patient is a dependent, as defined by the provisions of the National Health Insurance Act of 1995, of the 4Ps beneficiary member and is included in the NHTS-PR list of poor households; and
- Updated Member Data Record, if available
- IHCPs shall determine that the eligibility of a Pantawid Pamilya benificiary's coverage under the National Health Insurance Program (NHIP) whether as existing member or qualified dependent.
- PhilHealth CARES Nurses deployed in selected hospitals nationwide maybe tapped by the IHCPs for this purpose.
- IHCPs may use the IHCP Portal, which serves as a link between health care providers and PhilHealth through an online connection that will ensure verification of eligibility information of Sponsored Program Members identified under the NHTS-PR, per PhilHealth Circular No. 2, s. 2012 with subject: Guidelines on the Implementation of the IHCP Portal. For IHCPs who currently have no access to the IHCP Portal, the following Masterlists may be used:
- Softcopy/Hardcopy of Masterlist provided by PhilHealth Regional Offices;
- Web listing as reflected in www.philhealth.gov.ph/members/sponsored/nhts-pr_list.html
- For patient - Pantawid Pamilya ID Holder, with coverage as qualified dependent, the IHCP may check the name of the following in any of the Masterlists available, as applicable:
- If married, ask for the name of the spouse-member;
- If single, ask for age and the following:
- With age below 21 years old - ask for name of parent-member;
- With age above 60 years old - ask for then name of their child-member;
- For Pantawid Pamilya ID Holders who are determined to be unregistered to be unregistered members, entitlement to NHIP benefits shall still be provided to them and their qualified dependents.
- A fully accomplished Claim Form 1 (CF1), together with the photocopy of the Pantawid Pamilya ID Card, must be submitted by the IHCP, together with the required claim documents.
- In lieu of the PhilHealth Identification Number (PIN), the following remarks shall be indicated in the CF1: "Pantawid Pamilya for Registration".
- Also, the Civil Status and Sex/Gender of the Pantawid Pamilya Beneficiary shall be indicated on the space below the name of the Member (Part 1 - Member and Dependent Information, item number 3 of the PhilHealth Claim Form 1)
VI. CLAIMS PROCESSING
- For members with updated membership record, claims processing shall follow the usual procedures
- For members with PhilHealth Identification Number (PIN) but require updating of records, data reflected in submitted Claim Form 1 (CF1) shall be used as basis in amendment of records of Sponsored Program identified under the NHTS-PR.
- For members without PhilHealth Identification Number (PIN), data reflected in submitted Claim Forms shall be used for PIN generation and enrollment under the Sponsored Program under the NHTS-PR.
VII. EFFECTIVITY
This Circular shall take effect fifteen (15) days after publication in a newspaper of general circulation and shall be deposited thereafter with the National Administrative Register at the University of the Philippines Law Centre.
- https://www.affordablecebu.com/